Heart failure: A practical guide for congenital heart disease patients
It doesn't mean you're dying, but it's becoming more common. Here's what you need to know.
Welcome! This is The Heart Dialogues, a free newsletter for people born with heart conditions (and the people who care about them). Every other week, I’ll send you candid conversations, essays, guest posts and/or interesting links about what it’s really like to live with a weird and special heart. Join this community and support my work. Sign up for free.
Heart failure. What a terrible name. Taken together, the two words seem to hand down a death sentence, a confirmation of what you might have suspected would happen all along. My heart has failed. But…is that true?
“It does not mean your heart has failed. It doesn't mean that your heart is destined to fail. It also is not a terminal diagnosis,” said Luke J. Burchill, who leads the proactive adult congenital heart failure program at Mayo Clinic.
Is heart failure fun to read about? Not really. But it’s affecting more adults with CHD, simply because we’re living longer; the topic is riddled with myths and confusion; and the more you know about it, the better you can prevent and treat it.
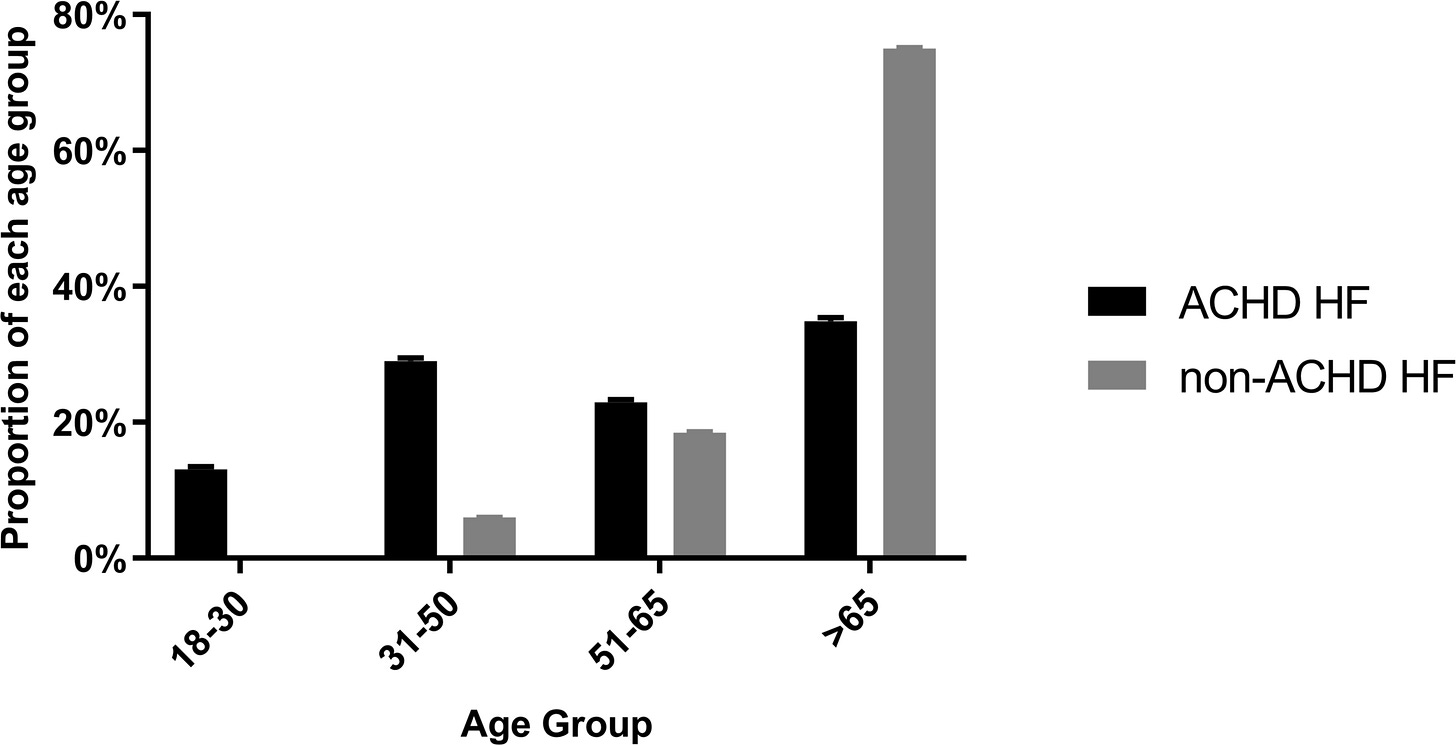
About 7.8% of CHD patients, or roughly one in 13, will develop heart failure, versus 1.1% in the general population, according to a 2022 study that looked at Swedish patient and death records to compare almost 90,000 CHD patients born between 1930 and 2017 against controls. Hospitalizations for CHD patients with heart failure more than doubled between 2010 and 2020, from 6.6% to 14%, even as total CHD hospitalizations remained stable, according to a 2023 study that looked at health-insurance claims for adults with CHD. Heart failure increases the risk of hospitalizations and death, and it’s the leading cause of death for adults with CHD, research shows.
But, crucially, heart failure is not a death sentence. Burchill, who was an author on the 2023 study, acknowledged how disorienting and scary a heart failure diagnosis can be, especially for people with CHD who might have dealt with heart issues all their lives. “It can be hugely impactful for a person and their family and their loved ones,” he said, “but what I'm saying is: Please don't give up hope and don't see it as a hopeless diagnosis.”
Note: I am not a doctor, and nothing in this should be taken as medical advice. I hope this guide is a jumping off point for conversations with your healthcare team.
What is heart failure?
Heart failure is a condition where the heart doesn’t pump enough blood to keep up with the body’s demands. That sounds simple, but it’s often more complicated for CHD patients.
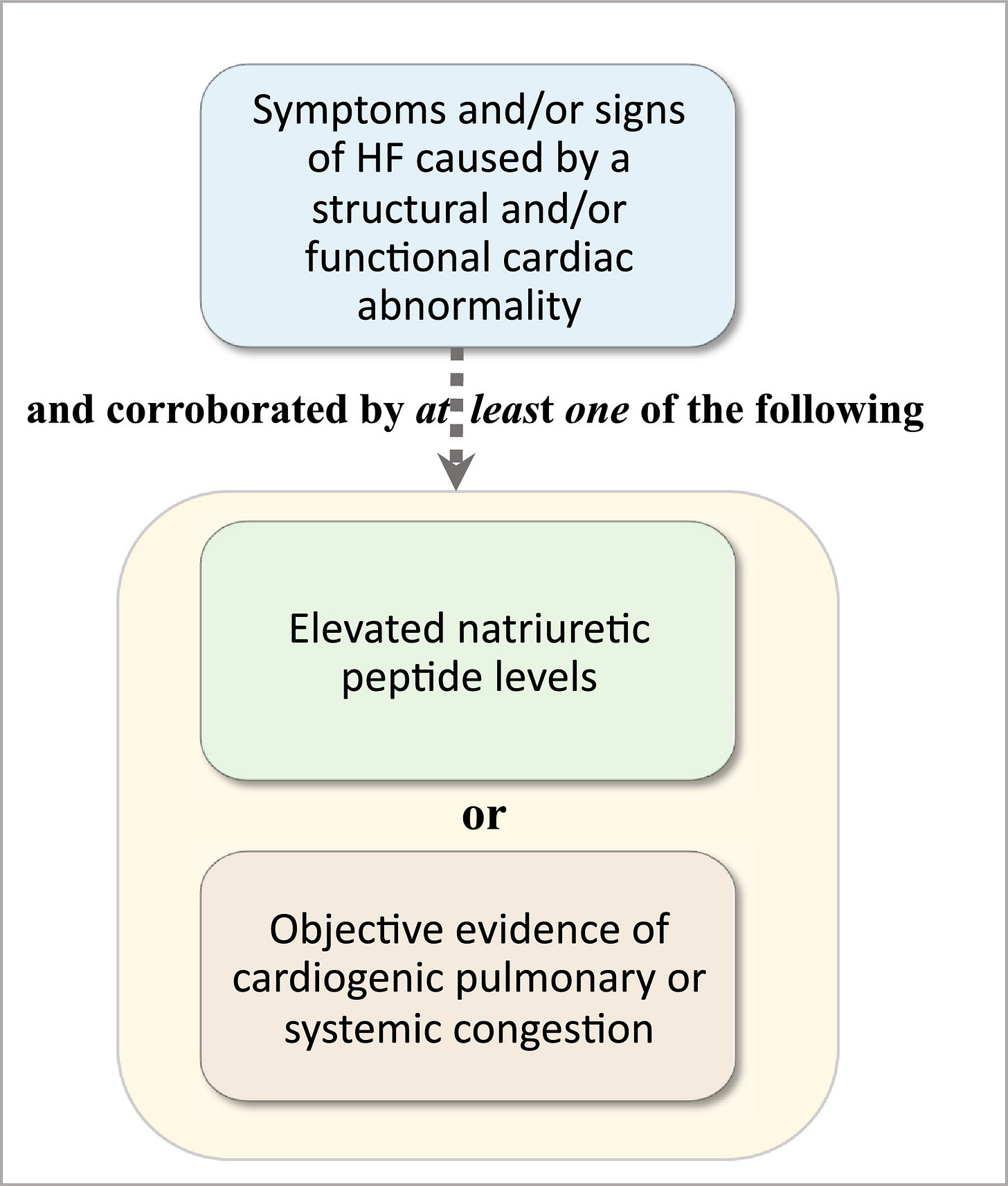
It’s also not black and white—as in, you’re in heart failure or you’re not. The American Heart Association and the American College of Cardiology use four stages of heart failure, from A to D. In later stages, the common New York Heart Association Functional Classification further divides into four classes based on physical activity limitations. In 2021, however, an international group of doctors proposed a new definition of heart failure that rests on three criteria: symptoms caused by altered heart function, congestion in the lungs or systemic veins, and elevated biomarkers, namely high levels of BNP (brain natriuretic peptide) and NT-proBNP (N-terminal prohormone of brain natriuretic peptide). (See below for more on diagnosing heart failure.)
What does heart failure feel like?
It’s possible to be in heart failure and not know anything is off, but classic symptoms include:
fatigue
shortness of breath
an inability to exercise
fluid retention
a cough that won’t go away
That means that tiredness is persistent without a good other explanation. Activities that used to be easy might become more difficult—at a faster rate than normal age-related decline. You might have swelling in your legs and/or belly, or feel out of breath when you lie down.
Allison, 52, has hypoplastic left heart syndrome, pulmonary hypertension and heart failure. She has had to reduce her work as an ESL tutor, make simpler meals, shop at smaller stores or online, and cut back on her social life in favor of reading or other solitary activities, she told me by email. “I feel I need to protect my energy like it is gold! If I wake up with a good amount of energy I know that it will not last, so I guard it to make sure I can do the things that are most important to me before I am on empty again,” she said.
You might also experience a range of emotions, including worry, dread, hypervigilance, anxiety or depression, especially if you aren’t able to do the things you once did, said Teresa Salinas, a cardiology social worker who works with CHD and heart failure patients at the Philadelphia Adult Congenital Heart Center.
“Doctors drop the bomb, ‘You have heart failure,’ and then seem surprised when we get upset. Worse, no support is offered,” one 40-year-old Alberta woman with congenital aortic stenosis and a pacemaker told me by email. “I have it, yet no one but me seems concerned.”

How is heart failure different for CHD patients?
The experience differs from those with acquired heart disease in several important ways.
It’s harder to diagnose.
First, the traditional stages don’t necessarily apply. The ACC/AHA guidelines put anyone with “structural heart disease” in Stage B, or “pre-heart failure.” That would apply to the vast majority of CHD patients without symptoms, according to a 2016 scientific statement from the AHA. And there isn’t enough evidence that categorizing CHD patients using these stages helps with care decisions or improves outcomes, the statement said.
It’s also more difficult to tell if CHD patients are experiencing symptoms. Exercise limitation is a classic sign of heart failure but also widespread among the CHD population. “Exercise limitation is sort of universal for the young adults that I see with congenital heart disease,” Burchill said, and it can be tricky to tease apart lifelong, multifactorial limitations from those that arise from the development of heart failure.
CHD patients often adapt to these limitations, so we might not report symptoms, even if our exercise ability is significantly impaired, the AHA statement said. In advanced heart failure, we also typically perform better on cardiopulmonary exercise tests—a common, objective diagnostic tool—than people with acquired heart disease, according to a 2022 review done by several Penn State cardiologists. For CHD patients, exercise testing might underestimate the severity of heart failure.
It doesn’t follow a typical trajectory.
Patients with acquired heart disease often progress slowly but predictably through the stages of heart failure. By contrast, CHD patients might spend years or even decades in heart failure, or between one episode of heart failure and another.
We get it younger.
Cardiologists who aren’t familiar with CHD might fail to diagnose heart failure because it shows up so much younger—at a mean age of 40.3 years old, compared with 66.4 years old in the general population, according to the study that looked at Swedish records. “When I see a patient who is 40 years old, they are basically a 66-year-old in terms of cardiovascular risk,” Curt Daniels, director of the adolescent and adult congenital heart disease program at Nationwide Children's Hospital, told the AHA.
This also means that we typically experience heart failure in different periods of our lives—perhaps in the midst of growing a family or climbing the career ladder, as opposed to the brink of retirement.
We are all unique.
Generally, treatment for heart failure comes down to which medication(s) patients take, and that is dictated by whether they have reduced or preserved ejection fraction, a measure of how much blood your heart is pumping, Burchill said. CHD patients, however, might have a wide array of cardiac anatomy—one ventricle or two? The left ventricle or the right? The diversity of conditions and anatomy make it difficult to do the big clinical trials that help illuminate the best courses of treatment, cardiologists said.
How is heart failure diagnosed in CHD patients?
It’s not like taking a Covid-19 test where one red line shows up if you’re negative and two red lines if you’re positive. No objective measure of heart failure applies to all CHD patients; subjective determinations by cardiologists are often involved. Two key components, though, are significant limitations in the ability to do regular activity and symptoms that are caused by the heart not pumping blood adequately, said Ari Cedars, director of the adult congenital heart disease center at Johns Hopkins.
Cardiologists use a variety of methods to diagnose heart failure, including clinical exams, exercise testing, imaging studies (like echocardiograms or MRIs) and lab values (obtained through blood work), Cedars said.
With exercise tests, patients might not be at the level of people with regular hearts, but cardiologists can see whether they fall outside the normal values for their conditions, Cedars said.
When it comes to lab values, cardiologists look at biomarkers, most commonly a hormone called brain natriuretic peptide, or BNP, which is an indicator of fluid retention, Cedars said. “The reason why that's a symptom of heart failure is because if your heart is not able to push enough blood through the kidneys, the kidneys interpret that as you being dehydrated and thereby cause you to retain water inappropriately. People with heart failure will frequently have fluid retention, which can be detected with a BNP,” Cedars said. There isn’t a threshold for BNP that says definitively that one patient is in heart failure and another one isn’t. But there are different thresholds for different conditions, Cedars said, and cardiologists also look at how BNP changes over time in individuals.

Who is at the greatest risk?
People with more complex congenital heart conditions are at the highest risk for developing heart failure, research shows.
Those with a group of heart defects including tetralogy of Fallot, transposition of the great arteries and double outlet right ventricle were about 42 times more likely to get heart failure than the general population, while a group including those with single ventricles, such as hypoplastic left heart syndrome and tricuspid atresia, were 21 times more likely, according to the study that looked at Swedish records. The risk was 8.7 times higher for CHD patients overall.
Another paper, the review by Penn State doctors, found that two groups are at a high risk for heart failure in adulthood: those with a systemic right ventricle and those with a single ventricle. By adulthood, heart failure shows up in 50% of those who’ve had the Fontan procedure, which is typically done to repair single-ventricle defects, the AHA statement said.
Can I prevent heart failure?
Possibly! While there aren’t long-term clinical trials to prove this definitively, some research suggests that eating a balanced diet heavy in fruits and vegetables, avoiding excessive salt intake and exercising regularly can help, Cedars said. Keeping your blood pressure under control and avoiding excessive alcohol use—meaning four to six drinks a day—might also help, Burchill said.
The single most important preventive measure? Regular cardiology care from a provider who’s familiar with CHD, Cedars said. You might have a leaking valve and not become symptomatic until things get bad. “And once things have gotten bad,” Cedars said, “the probability they're reversible is much lower.”
Can I reverse heart failure?
In some cases, yes.
The root cause
Heart failure in CHD patients sometimes has an identifiable, addressable cause, such as an arrhythmia (heart rhythm problem), valve issues or an infection. Tackling that cause, whether through medications or a procedure, can stop heart failure. In fact, the onset of heart failure can sometimes be a signal that it’s time to replace a valve or pursue another intervention, Burchill said. “I would always start with the question of why,” he said. “Why have I developed heart failure now?”
Medication
Some medications have been demonstrated to potentially reverse heart failure in the general heart-disease population, and they probably work in some forms of CHD as well, Cedars said. (See more below.)
Lifestyle changes
No lifestyle change has been proven to reverse heart failure, but exercise and salt restriction could help, Cedars said. Ask your cardiologist about how vigilant you should be about salt intake, if at all—advice tends to vary patient to patient and provider to provider. As for exercise, Cedars recommends a moderate level of activity—getting your heart rate between 60% to 80% of its maximum—for 30 minutes five times a week. Resistance training can be helpful too, but check with your cardiologist first. (Remember, no one is obligated to exercise!)
Allison said she goes on half-mile walks with her dogs several times a day, weather permitting. “I try to average four walks a day, when possible. I take my time, and it can be difficult sometimes, but I don’t want to stop as I feel it is very helpful and the doctor agrees,” she said.

What medications treat heart failure?
No proven medical therapy exists for heart failure in adults with CHD, but drugs that help the general heart failure population are likely to help CHD patients. This is particularly true for people whose hearts are closer to regular cardiac anatomy, such as those with atrial or ventricular septal defects (holes in the heart) or tetralogy of Fallot, Cedars said.
According to Cedars, medications fall into four pillars of treatment. Feel free to take this list to your next appointment and ask your cardiologist if any of these medications might apply to you.
beta blockers, including metoprolol
renin-angiotensin system blockers, or RAS blockers, including Entresto (which is a specific kind of RAS blocker)
mineralocorticoid receptor antagonists, including spironolactone and eplerenone
sodium-glucose cotransporter-2 inhibitors, or SGLT-2 inhibitors, including Farxiga and Jardiance
Which medications you take, if any, will come down to your specific anatomy and situation, as well as the philosophy of your cardiologist. “It becomes a stylistic thing. Some providers will say, ‘Well, we don't know if it's proven, but it may help. I'm going to just put all my patients on it,’” Cedars said. “Some people say, ‘Well, based on the mechanism of action, I think this one may be beneficial and that one may not be.’ You'll see a lot of variation from provider to provider in which drugs they choose to use in which groups of patients.”
Lastly, diuretics are a common medication to alleviate symptoms of heart failure, though they don’t treat the condition itself. Also known as water pills, diuretics help the body pee out water and salt, lowering the amount of fluid in the veins and arteries and reducing blood pressure.
Are there other treatment options?
Ventricular assist devices, or implantable devices that essentially take over the pumping function of the heart, represent an emerging area of treatment for CHD patients in advanced heart failure. While they are far more common among the general heart-failure population, they are becoming more popular for those with CHD, with some people receiving VADs as “destination therapy” instead of a bridge to a heart transplant, Cedars said.
They’re not a magic bullet. They won’t work for all CHD patients. Left ventricular assist devices, for example, are designed to work in place of a left ventricle, which some CHD patients don’t have. Knowing when to implant one is tricky, too. Do it too early, and the devices might develop problems—it isn’t clear how long they last. Do it too late, and patients might not be healthy enough, potentially leading to complications. Yet another heart surgery for people who might have already had several can make an eventual transplant more difficult, Cedars said. And today’s machines need to get power through a cord that hangs out of the chest, which has to be plugged into batteries that must be carried everywhere, he said.
When is a heart transplant needed?
A diagnosis of heart failure does not mean the next step is a heart transplant. Transplants are an option for patients with severe, advanced heart failure that continues despite medical and surgical treatments. In other words, patients are going in and out of the hospital, fluid buildup or rhythm problems persist despite medication adjustments or procedures, and/or heart failure is affecting other organs such as the kidneys, lungs, liver or brain, Burchill said.
“We really think about transplant when someone presents and we say, ‘Wow, they've got a number of complications arising from heart failure that limit their survival over the next year or two—not three, four or five—really, over the next 12 months,” Burchill said.
Heart transplants should be done at specialized centers for the best outcomes, Cedars said.
How can I cope with my emotions?
It’s natural to be scared or unsure after a diagnosis of heart failure (or worry if a diagnosis might come someday). Some people, particularly those who are younger, fear for the future. “What if I don't make it to such and such an age? Or what if I am going to get worse really soon and I'm not able to do the things that I enjoy, like being around my children or my grandchildren?” Salinas said. Others, particularly those in their 60s or 70s who might have had earlier generations of surgical repairs, might be at peace with the diagnosis, Salinas said.
Some CHD centers have mental-healthcare providers on staff, who can help with more than you might expect. Salinas said she provides patients with short-term counseling and connects them with therapists, but she also helps them navigate care, consults on insurance and affordability questions, and helps them access disability benefits.
Think about the other tools in your toolbox, Salinas recommends. That might include people you can talk to, activities that you enjoy, mindfulness exercises or breathwork, peer-to-peer support, addressing sleep issues, additional visits with your cardiologist to get more information, or medications, she said.
Heart failure focuses on the deficits, but Burchill said he likes to think about the strengths his patients bring to the table, whether that’s the ability to consistently take medication, a deep bench of supportive friends or the motivation to exercise. “My heart may be failing,” he said, “but it doesn't mean that I am a failure.”
Resources
Classes and Stages of Heart Failure. The American Heart Association lays it out.
ACHD and Heart Failure Webinar. In this 50-minute session from the Adult Congenital Heart Association, Ari Cedars of Johns Hopkins goes over the basics of heart failure for adults with CHD.
ACHD and Heart Failure YouTube Series. Mayo Clinic’s Luke Burchill dives into heart failure and CHD, among other topics, in this collection of video clips, most under three minutes.
Coping + Getting Help Deck. This presentation compiled by cardiology social worker Teresa Salinas offers dozens of practical tips for CHD patients dealing with tough times.



You have done it again with this article. That has been a dreaded term in our CHD family, but we learned too it could be managed. Yes. Let’s work on rebranding the term and increasing awareness with articles such as this.
As a nurse practitioner with an adult child with CHD associated heart failure this article is spot on. Excellent job and thank you for your work. I look forward to reading more!